Mental health and well being

Maintaining a healthy mental outlook during the COVID-19 pandemic is equally as important as taking physical measures to stop the spread of the virus.
The current events and news surrounding global COVID-19 are understandably affecting, in different ways for each of us, our mental health and wellbeing. Many in our community are feeling distressed, and at times overwhelmed, by what is happening to them, their families and their community.
Feeling confused and uncertain about the future is a normal, understandable reaction at a time like this. We all have different ways of coping, but one important aspect of how we cope is to remember that we are not alone in how we feel.
It is important to know that you are not alone and there are people and services that can give you the help, support and assistance you need.
Tips on maintaining good mental health
• Make sure you maintain your daily routine as much as possible including regular exercise and a good sleep pattern.
• Talk to other members of your family, friends or colleagues about the infection. Understanding COVID-19 can reduce anxiety.
• Think about how much media and social media you are accessing. Constantly watching or listening to information about distressing events can make things feel worse.
• Be kind to yourself and don’t expect to have all the answers, difficult though that might be.
Tips for those who are in quarantine or isolation
• Maintain a positive attitude. Think about how you’ve managed in other difficult situations and reassure yourself that you will cope with this situation as well. Home quarantine is only temporary.
• Reassure children using age-appropriate language.
• If at home with others, consider everyone’s needs including have some time alone during the day.
• Accept that conflict and arguments may occur. Try to resolve them as soon as possible. For young children, distraction may help.
• Stay in touch with family members and friends by phone, email or social media.
• Exercise regularly at home as it helps to reduce stress. Options include yoga, floor exercises, dancing, exercise DVDs or online videos, and walking around the backyard
Social Stigma associated with COVID-19
WHAT IS SOCIAL STIGMA?
Social stigma in the context of health is the negative association between a person or group of people who share certain characteristics and a specific disease. In an outbreak, this may mean people are labelled, stereotyped, discriminated against, treated separately, and/or experience loss of status because of a perceived link with a disease.
Such treatment can negatively affect those with the disease, as well as their caregivers, family, friends and communities. People who don’t have the disease but share other characteristics with this group may also suffer from stigma.
The current COVID-19 outbreak has provoked social stigma and discriminatory behaviours against people of certain ethnic backgrounds as well as anyone perceived to have been in contact with the virus.
WHY IS COVID-19 CAUSING SO MUCH STIGMA?
The level of stigma associated with COVID-19 is based on three main factors:
1. It is a disease that’s new and for which there are still many unknowns;
2. We are often afraid of the unknown; and
3. It is easy to associate that fear with ‘others’. It is understandable that there is confusion, anxiety, and fear among the public. Unfortunately, these factors are also fueling harmful stereotypes.
WHAT IS THE IMPACT?
Stigma can undermine social cohesion and prompt possible social isolation of groups, which might contribute to a situation where the virus is more, not less, likely to spread. This can result in more severe health problems and difficulties controlling a disease outbreak.
Stigma can:
- Drive people to hide the illness to avoid discrimination
- Prevent people from seeking health care immediately
- Discourage them from adopting healthy behaviours
HOW TO ADDRESS SOCIAL STIGMA?
Evidence clearly shows that stigma and fear around communicable diseases hamper the response. What works is building trust in reliable health services and advice, showing empathy with those affected, understanding the disease itself, and adopting effective, practical measures so people can help keep themselves and their loved ones safe. How we communicate about COVID-19 is critical in supporting people to take effective action to help combat the disease and to avoid fuelling fear and stigma. An environment needs to be created in which the disease and its impact can be discussed and addressed openly, honestly and effectively.
Here are some tips on how to address and avoid compounding, social stigma:
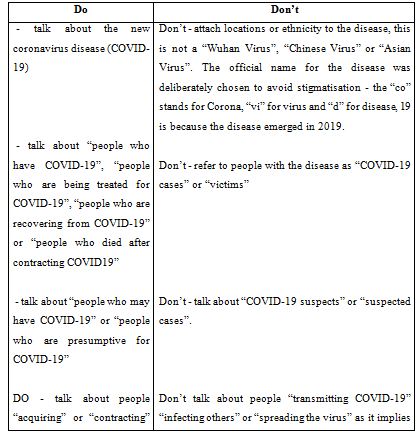
1. Words matter: dos and don’ts when talking about the new coronavirus (COVID-19)
2. Do your part: simple ideas to drive stigma away
3. Communication tips and messages.
1. WORDS MATTER:
When talking about coronavirus disease, certain words (i.e suspect case, isolation…) and language may have a negative meaning for people and fuel stigmatizing attitudes. They can perpetuate existing negative stereotypes or assumptions, strengthen false associations between the disease and other factors, create widespread fear, or dehumanise those who have the disease.
This can drive people away from getting screened, tested and quarantined. We recommend a ‘peoplefirst’ language that respects and empowers people in all communication channels, including the media. Words used in media are especially important, because these will shape the popular language and communication on the new coronavirus (COVID-19). Negative reporting has the potential to influence how people suspected to have the new coronavirus (COVID-19), patients and their families and affected communities are perceived and treated.
2. DO YOUR PART:
Governments, citizens, media, key influencers and communities have an important role to play in preventing and stopping stigma surrounding people. We all need to be intentional and thoughtful when communicating on social media and other communication platforms, showing supportive behaviors around the new coronavirus disease (COVID-19).
Here are some examples and tips on possible actions to counter stigmatizing attitudes:
- Spreading the facts: Stigma can be heightened by insufficient knowledge about how the new coronavirus disease (COVID-19) is transmitted and treated, and how to prevent infection. In response, prioritise the collection, consolidation and dissemination of accurate community-specific information about affected areas, individual and group vulnerability to COVID19, treatment options and where to access health care and information. Use simple language and avoid clinical terms. Social media is useful for reaching a large number of people with health information at relatively low cost.
- Engaging social influencers : such as religious leaders on prompting reflection about people who are stigmatized and how to support them, or respected celebrities to amplify messages that reduce stigma. The information should be well targeted and the celebrities who are asked to communicate this information must be personally engaged, and geographically and culturally appropriate to the audiences they seek to influence. An example would be a mayor (or another key influencer) going live on social media and shaking hands with the leader of the Chinese community.
- Amplify the voices, stories and images of local people who have experienced the new coronavirus (COVID-19) and have recovered or who have supported a loved one through recovery to emphasise that most people do recover from COVID-19. Also, implementing a “hero” campaign honouring caretakers and healthcare workers who may be stigmatized. Community volunteers also play a great role in reducing stigma in communities.
- Make sure you portray different ethnic groups. All materials should show diverse communities being impacted and working together to prevent the spread of COVID-19. Ensure that typeface, symbols and formats are neutral and don’t suggest any particular group.
- Ethical journalism: Journalistic reporting which overly focuses on individual behaviour and patients’ responsibility for having and “spreading COVID-19” can increase stigma of people who may have the disease. Some media outlets have, for example, focused on speculating on the source of COVID-19, trying to identify “patient zero” in each country. Emphasizing efforts to find a vaccine and treatment can increase fear and give the impression that we are powerless to halt infections now. Instead, promote content around basic infection prevention practices, symptoms of COVID-19 and when to seek health care.
- Link up: There are a number of initiatives to address stigma and stereotyping. It is key to link up to these activities to create a movement and a positive environment that shows care and empathy for all.
3. COMMUNICATION TIPS and MESSAGES
An “infodemic” of misinformation and rumours is spreading more quickly than the current outbreak of the new coronavirus (COVID-19). This contributes to negative effects including stigmatization and discrimination of people from areas affected by the outbreak. We need collective solidarity and clear, actionable information to support communities and people affected by this new outbreak.
Misconceptions, rumours and misinformation are contributing to stigma and discrimination which hamper response efforts.
- Correct misconceptions, at the same time as acknowledging that people’s feelings and subsequent behaviour are very real, even if the underlying assumption is false.
- Promote the importance of prevention, lifesaving actions, early screening and treatment.
Collective solidarity and global cooperation are needed to prevent further transmission and alleviate the concerns of communities.
- Share sympathetic narratives, or stories that humanize the experiences and struggles of individuals or groups affected by the new coronavirus (COVID-19)
- Communicate support and encouragement for those who are on the frontlines of response to this outbreak (health care workers, volunteers, community leaders etc).
Facts, not fear will stop the spread of novel coronavirus (COVID-19)
- Share facts and accurate information about the disease.
- Challenge myths and stereotypes.
- Choose words carefully. The way we communicate can affect the attitudes of others.
Basic protective measures against the new coronavirus
Take care of your health and protect others by doing the following:
Wash your hands frequently: Regularly and thoroughly clean your hands with an alcohol-based hand rub or wash them with soap and water.
Why? Washing your hands with soap and water or using alcohol-based hand rub kills viruses that may be on your hands.
Maintain social distancing: Maintain at least 1 metre (3 feet) distance between yourself and anyone who is coughing or sneezing.
Why? When someone coughs or sneezes they spray small liquid droplets from their nose or mouth which may contain virus. If you are too close, you can breathe in the droplets, including the COVID-19 virus if the person coughing has the disease.
Avoid touching eyes, nose and mouth
Why? Hands touch many surfaces and can pick up viruses. Once contaminated, hands can transfer the virus to your eyes, nose or mouth. From there, the virus can enter your body and can make you sick.
Practice respiratory hygiene: Make sure you, and the people around you, follow good respiratory hygiene. This means covering your mouth and nose with your bent elbow or tissue when you cough or sneeze. Then dispose of the used tissue immediately.
Why? Droplets spread virus. By following good respiratory hygiene you protect the people around you from viruses such as cold, flu and COVID-19.
If you have fever, cough and difficulty breathing, seek medical care early: Stay home if you feel unwell. If you have a fever, cough and difficulty breathing, seek medical attention and advance. Follow the directions of your local health authority.
Why? National and local authorities will have the most up to date information on the situation in your area. Calling in advance will allow your health care provider to quickly direct you to the right health facility. This will also protect you and help prevent spread of viruses and other infections.
Stay informed and follow advice given by your healthcare provider
Stay informed on the latest developments about COVID-19. Follow advice given by your healthcare provider, your national and local public health authority or your employer on how to protect yourself and others from COVID-19.
Why? National and local authorities will have the most up to date information on whether COVID-19 is spreading in your area. They are best placed to advise on what people in your area should be doing to protect themselves.
Stay at home if you begin to feel unwell, even with mild symptoms such as headache and slight runny nose, until you recover.
Why? Avoiding contact with others and visits to medical facilities will allow these facilities to operate more effectively and help protect you and others from possible COVID-19 and other viruses.
If you develop fever, cough and difficulty breathing, seek medical advice promptly as this may be due to a respiratory infection or other serious condition.
Why? Calling in advance will allow your health care provider to quickly direct you to the right health facility. This will also help to prevent possible spread of COVID-19 and other viruses.
'You must always return to yourself.'
With many healthcare workers around the world stretched by demand, how can they deal with emotions and stress?
Many consultants have headaches and nausea when they deal with stress and emotion,. "Consultants are easily overly involved and fall into a sense of powerlessness."
There are also times when there is nothing they can do. For example, at times, they cannot provide beds, masks and other needed supplies. In times like these, psychological counselling for crisis intervention tests the personal growth and skill of a consultant.
"You must always return to yourself, be aware of yourself, and distinguish which emotions are yours, which are the patients, and which are your empathy,".
'Think about mental health as part of the public health response.'
“It’s really important to think about mental health as part of the public health response to COVID-19."
"People who might be vulnerable to experiencing stress during this time might include people who have preexisting mental health conditions, or substance use conditions, or who might represent other vulnerable groups. I am not just talking about protection from COVID-19, but also talking about prevention of stress and fear during this event.”
We need to do:
- Integration of key messages related to mental health and stigma in the training material of frontline workers from health and non-health sectors; the training of the national COVID-19. The Ministry of Public Health (MOPH) guidelines to the public on self-isolation, including on social media; and the communication messages targeting the general public, health care workers, and others
- Development of a social media campaign on mental health targeting the general population, caregivers of children, persons in self-isolation, and workplaces to support employees with flexible work arrangements
- Self-care and support for health care staff and front-liners during this period
- On-call, phone-based mental health support for persons in quarantine
'Social isolation is associated with poor mental health.'
The social causes of health, mental health and trauma, does not dismiss the risk of spread of the novel coronavirus, but it's also important to consider unexpected risks associated with the response to the outbreak. “The fact that social isolation is associated with poor mental health is unquestionable,” .
In addition, macro-level stress across society could have an the Poor and Marginalized Will Be the Hardest Hit by Coronavirus (undue social burden on specific populations). "There will be medium and long-term consequences on people whose employment is in sectors like retail and transportation" "Adding economic pressures will inevitably result in worse mental health.”
The effects of quarantining on people’s mental health. Those quarantined displayed symptoms of post-traumatic stress disorder and depression.
If quarantining is necessary, there are steps that can mitigate the effects of being isolated, including:
• Staying connected with your social and family networks via technology
• Keeping your daily routines as much as possible
• Exercising regularly and practicing habits that you enjoy and find relaxing
• Seeking practical, credible information at specific times of the day
How to handle your mental health during the pandemic COVID-19 Anxiety
The unfortunate thing about fear is it also is contagious and when we see other people responding with fear and anxiety, we tend to respond the same way,
Advice for those feeling their anxiety increase as the virus continues to spread:
- Trust decision makers and the tactics and strategies they're advising us to follow.
- Stay healthy by getting enough sleep, eating healthy, and exercising
- Practice social distancing
- Limit social media consumption
Mental Health and Psychosocial Considerations During COVID-19 Outbreak
The World Health Organization (WHO) declared the outbreak of a new coronavirus disease to be a Public Health Emergency of International Concern. WHO stated there is a high risk of the 2019 coronavirus disease (COVID-19) spreading to other countries around the world.
WHO made the assessment that COVID-19 can be characterized as a pandemic. WHO and public health authorities around the world are acting to contain the COVID-19 outbreak. However, this time of crisis is generating stress in the population. The mental health considerations Use as messages targeting different groups to support for mental and psychosocial well-being during COVID-19 outbreak.
General population
- COVID-19 has and is likely to affect people from many countries, in many geographical locations. Do not attach it to any ethnicity or nationality. Be empathetic to all those who are affected. People who are affected by Covid-19 have not done anything wrong, and they deserve our support, compassion and kindness.
- Do not refer to people with the disease as “COVID-19 cases”, “victims” “COVID-19 families” or the “diseased”. They are “people who have COVID-19”, “people who are being treated for COVID19”, “people who are recovering from COVID-19” and after recovering from COVID-19 their life will go on with their jobs, families and loved ones. It is important to separate a person from having an identity defined by COVID-19, to reduce stigma.
- Minimize watching, reading or listening to news that causes you to feel anxious or distressed; seek information only from trusted sources and mainly to take practical steps to prepare your plans and protect yourself and loved ones. Seek information updates at specific times during the day, once or twice. The sudden and near-constant stream of news reports about an outbreak can cause anyone to feel worried. Get the facts; not the rumors and misinformation. Facts can help to minimize fears.
- Protect yourself and be supportive to others. Assisting others in their time of need can benefit the person receiving support as well as the helper.
- Find opportunities to amplify positive and hopeful stories and positive images of local people who have experienced COVID-19. For example, stories of people who have recovered or who have supported a loved one and are willing to share their experience.
- Honor caretakers and healthcare workers supporting people affected with COVID-19 in your community. Acknowledge the role they play to save lives and keep your loved ones safe.
Healthcare workers
- For health workers, feeling under pressure is a likely experience for you and many of your health worker colleagues. It is quite normal to be feeling this way in the current situation. Stress and the feelings associated with it are by no means a reflection that you cannot do your job or that you are weak. Managing your mental health and psychosocial wellbeing during this time is as important as managing your physical health.
- Take care of yourself at this time. Try and use helpful coping strategies such as ensuring sufficient rest and respite during work or between shifts, eat sufficient and healthy food, engage in physical activity, and stay in contact with family and friends. Avoid using unhelpful coping strategies such as tobacco, alcohol or other drugs. In the long term, these can worsen your mental and physical wellbeing. This is a unique and unprecedent scenario for many workers, particularly if they have not been involved in similar responses. Even so, using strategies that have worked for you in the past to manage times of stress can benefit you now. You are most likely to know how to de-stress and you should not be hesitant in keeping yourself psychologically well.
- Some healthcare workers may unfortunately experience avoidance by their family or community due to stigma or fear. This can make an already challenging situation far more difficult. If possible, staying connected with your loved ones including through digital methods is one way to maintain contact. Turn to your colleagues, or other trusted persons for social support- your colleagues may be having similar experiences to you.
- Use understandable ways to share messages with people with intellectual, cognitive and psychosocial disabilities. Forms of communication that do not rely solely on written information should be utilized If you are a team leader or manager in a health facility.
- Know how to provide support to, for people who are affected with COVID-19 and know how to link them with available resources. This is especially important for those who require mental health and psychosocial support. The stigma associated with mental health problems may cause reluctance to seek support for both COVID-19 and mental health conditions. clinical guidance for addressing priority mental health conditions and is designed for use by general health workers.
Team leaders or managers in health facility
- Keeping all staff protected from chronic stress and poor mental health during this response means that they will have a better capacity to fulfill their roles. Be sure to keep in mind that the current situation will not go away overnight and you should focus on longer term occupational capacity rather than repeated short-term crisis responses.
- Ensure good quality communication and accurate information updates are provided to all staff. Rotate workers from higher-stress to lower-stress functions. Partner inexperienced workers with their more experienced colleagues. The organization system helps to provide support, monitor stress and reinforce safety procedures. Ensure that outreach personnel enter the community in pairs. Initiate, encourage and monitor work breaks. Implement flexible schedules for workers who are directly impacted or have a family member impacted by a stressful event. Ensure you build in time for colleagues to provide social support to each other.
- If you are a team leader in a health facility, facilitate access to, and ensure staff are aware of where they can access mental health and psychosocial support services. Team leaders are also facing similar stressors as their staff, and potentially additional pressure in the level of responsibility of their role. It is important that the above provisions and strategies are in place for both workers and team leader, and can be a role-model of self-care strategies to mitigate stress.
- Orient responders, including nurses, ambulance drivers, volunteers, case identifiers, teachers and community leaders and workers in quarantine sites, on how to provide basic emotional and practical support to affected people using psychological first aid
- Manage urgent mental health and neurological complaints (e.g. delirium, psychosis, severe anxiety or depression) within emergency or general health care facilities. Appropriate trained and qualified staff may need to be deployed to these locations when time permits, general health care staff capacity in mental health and psychosocial support should be increased.
- Ensure availability of essential, generic psychotropic medications at all levels of health care. People living with long-term mental health conditions or epileptic seizures will need uninterrupted access to their medication, and sudden discontinuation should be avoided.
Care providers for children
- Help children find positive ways to express feelings such as fear and sadness. Every child has their own way to express emotions. Sometimes engaging in a creative activity, such as playing, and drawing can facilitate this process. Children feel relieved if they can express and communicate their feelings in a safe and supportive environment.
- Keep children close to their parents and family, if considered safe for the child, and avoid separating children and their caregivers as much as possible. If a child needs to be separated from their primary caregiver, ensure that appropriate alternative care is provided and that a social worker, or equivalent, will regularly follow up on the child.
- Maintain familiar routines in daily life as much as possible, or create new routines, especially if children must stay at home. Provide engaging age appropriate activities for children, including activities for their learning. As much as possible, encourage children to continue to play and socialize with others, even if only within the family when advised to restrict social contract.
- During times of stress and crisis, it is common for children to seek more attachment and be more demanding on parents. Discuss COVID-19 with your children using honest and ageappropriate way. If your children have concerns, addressing those together may ease their anxiety. Children will observe adults’ behaviors and emotions for cues on how to manage their own emotions during difficult times.
Older adults, care providers and people with underlying health conditions
- Older adults, especially in isolation and those with cognitive decline/dementia, may become more anxious, angry, stressed, agitated, and withdrawn during the outbreak/while in quarantine. Provide practical and emotional support through informal networks (families) and health professionals.
- Share simple facts about what is going on and give clear information about how to reduce risk of infection in words older people with/without cognitive impairment can understand. Repeat the information whenever necessary. Instructions need to be communicated in a clear, concise, respectful and patient way. It may also be helpful for information to be displayed in writing or pictures. Engage their family and other support networks in providing information and helping them practice prevention measures (e.g. handwashing etc.)
- If you have an underlying health condition, make sure to have access to any medications that you are currently using. Activate your social contacts to provide you with assistance, if needed.
- Be prepared and know in advance where and how to get practical help if needed.
- Learn simple daily physical exercises to perform at home, in quarantine or isolation to maintain mobility and reduce boredom.
- Keep regular routines and schedules as much as possible or help create new ones in a new environment, including regular exercising, cleaning, daily chores, singing, painting or other activities. Help others, through peer support, neighbor checking, and childcare for medical personnel restricted in hospitals fighting against COVID-19 when safe to do so. in accordance with previous ones. Keep regular contact with loved ones (e.g. via phone or other accesses).
People in isolation
- Stay connected and maintain your social networks. Even when isolated, try as much as possible to keep your personal daily routines or create new routines. If health authorities have recommended limiting your physical social contact to contain the outbreak, you can stay connected via e-mail, social media, video conference and telephone.
- During times of stress, pay attention to your own needs and feelings. Engage in healthy activities that you enjoy and find relaxing. Exercise regularly, keep regular sleep routines and eat healthy food.
- A near-constant stream of news reports about an outbreak can cause anyone to feel anxious or distressed. Seek information updates and practical guidance at specific times during the day from health professionals and avoid listening to or following rumors that make you feel uncomfortable.
Bir hospital Nursing Campus
NAMS Faculty



_rcn1YzUXpY.jpg)




Leave Comment